It’s hard to understate the importance of our immune system in our everyday health. While we’re out attending to our daily responsibilities, our immune system stays on constant lookout for dangerous invaders. In most cases, our bodies’ defense systems have an excellent batting average when it comes to eliminating hostile threats. Of the millions of microscopic bacteria, virus cells and other toxins that enter our bloodstream, only a tiny few manage to actually cause us to fall ill. Though its normal to take it for granted, the immune system is one of the body’s key mechanisms that make daily life possible.
But what if this highly effective security system malfunctioned, and wound up attacking the very body it is meant to protect? Sadly, this is hardly an unheard of problem. In fact, such ailments even have their own classification, known as autoimmune diseases. One particularly troublesome autoimmune condition is the ominous-sounding Graves’ disease, which afflicts the body’s thyroid gland. As with other autoimmune maladies, a cure for Graves’ disease has yet to be unearthed, although current treatment methods can mitigate the hallmark symptoms of this condition.
Too Much of a Good Thing
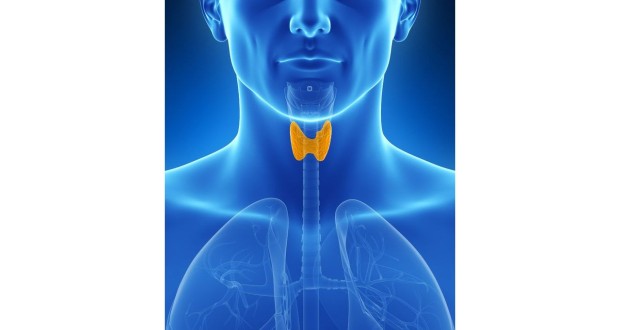
In the lower front part of your neck lies the thyroid, a butterfly-shaped gland tasked with producing specific hormones called thyroxine and triiodothyronine (these chemicals are also referred to as T-4 and T-3 hormones, respectively). These two hormones manage your metabolism and body temperature, while also contributing to the creation of new proteins (the body uses such proteins to manufacture new cells).
Though they play an essential role in your overall health, an overabundance of T3 and T4 hormones can cause a number of seemingly inexplicable problems to appear. In some patients, the thyroid gland gets stuck in overdrive, producing far more hormones than the body needs. Consequentially, the body’s metabolism is likewise forced to operate at an abnormally fast rate, causing the patient to experience a pounding heart, bouts of sweating and trembling. This lighting-quick metabolism quickly burns through all incoming foods and drinks, causing the patient to experience a noticeable drop in weight.
The culprit behind this sudden spike in thyroid activity isn’t a foreign virus or bacteria strain. Rather, Graves’ disease arises when the body’s immune system begins to unnecessarily produce certain types of antibodies, or proteins designed to neutralize or eliminate harmful toxins. In this case, the antibodies in question appear indistinguishable from a chemical known as TSH. This wouldn’t be a problem, except that TSH is the used by the brain to place its orders for hormones from the thyroid. The thyroid gland mistakes these antibodies for TSH signals, and proceeds to up its hormonal output.
The Many Symptoms of Graves’ Disease
Since the thyroid’s hormones impact so many aspects of our health, it makes sense that the problems associated with Graves’ disease are wide-ranging in their effect. Everything from the patient’s eyes, skin and even waistline can suffer the consequences of these extraneous thyroid hormones. People diagnosed with Graves disease typically exhibit at least of the following symptoms:
A significant loss in weight despite an increasingly strong appetite
- Accelerated heart rate
- Higher blood pressure readings
- Feelings of nervousness and anxiety
- Bowel movements occur more often
- Muscles throughout the body feel weak and fatigued
- Trembling hands
- The patient’s eyes bulge outward
- The skin covering the shins (the area between the knee joint and ankle) turns red and develops a thick and lumpy texture
- Women with Graves’ disease may experience menstrual periods on a less frequent basis; some female patients may stop having them altogether
Treatment Options
The logical course of action for treating patients with Grave’s disease is to bring the thyroid back under control. To achieve this goal, doctors frequently prescribe radioactive iodine. Despite its intimidating name, radioactive iodine therapy is fairly straightforward process; the patient simply swallows a capsule or drink containing this medicine. Once inside the body, radioactive iodine eliminates the excessive T3 and T4 hormones produced by the thyroid.
After ingesting radioactive iodine, people are strongly discouraged from kissing or engaging in any intimate contact for 24 hours, and are also told to largely avoid pregnant women and children for five days following treatment. To ensure that this medication is succinctly discharged from the body, patients are urged to drink at least four glasses of water daily.
In lieu of radioactive iodine, the doctor might instead advise the use of other medications that limit the thyroid’s hormonal production. Two of the most popular alternatives are propylthiouracil and methimazole. Anti-thyroid drugs can be taken either before or after the patient undergoes radioactive therapy. Some patients respond well to a third treatment option known as beta blockers. Rather than confronting extraneous thyroid hormones directly, beta blockers work to counteract the effects of these chemicals, thereby reducing or even curing the symptoms of Graves’ disease.
In a relatively small number of cases, most of the thyroid must be surgically removed to relieve the patient’s symptoms. If the eyes have become noticeably swollen, reddened or painful, the patient may be prescribed a combination of artificial tears and lubricating gels. Should these issues prove especially persistent or severe, other treatments may be necessary, including corticosteroids, eye muscle surgery or surgery to remove bone between the eye socket and sinuses (this procedure is known as orbital decompression surgery).
Although its name may indicate otherwise, the prognosis for Graves’ patients is actually fairly good, as most react favorably to treatment. A few complications might develop due to a patient’s medication, however. Hypothyroidism, a condition in which the body’s supply of thyroid hormones declines to insufficient levels, can occur in those who receive radioactive iodine or undergo thyroid surgery. This side effect can usually be prevented with thyroid hormone replacements.
 Natural Knowledge 24/7 Educate yourself with nutrition, health and fitness knowledge.
Natural Knowledge 24/7 Educate yourself with nutrition, health and fitness knowledge.