Never heard of deep vein thrombosis (DTV)? You’re hardly alone; a 2002 survey found that 74% of Americans knew little or absolutely nothing about this condition. This obscurity shouldn’t be taken to mean that DTV has a minor impact on public health. Each year, roughly two million Americans develop deep vein thrombosis, and an estimated 300,000 die from DTV-related complications. Though deep vein thrombosis certainly poses a major threat to the human body, taking the proper precautions can make it significantly less likely to appear.
The Downside of Blood Clotting
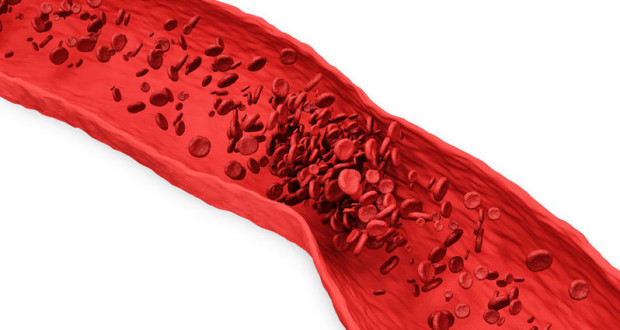
If you’ve ever had a cut (which covers just about everyone), then you’ve seen blood clotting in action. In short, the term “clot” refers to when blood hardens and congeals, transforming from a liquid into a solid state. Blood clots are one of the body’s most important self-repairing mechanisms; without them, there would be nothing to stop blood from endlessly pouring out of a wound.
Unfortunately, blood clots can also be dangerous in certain situations. A clot that forms inside a vein is known as a thrombus. Usually, thrombi form in response to internal damage, and are dissolved when the injury has sufficiently healed. In some cases, however, thrombi develop when they are not needed. If these clots grow large enough in size, they can obstruct the flow of blood through the vein.
The Role of Deep Veins
Not all veins have the same characteristics and responsibilities. In fact, there are four types of veins within the body, known as systematic, pulmonary, superficial and deep veins. As their name suggests, deep veins are found far underneath the skin, positioned deeply inside various muscles. Of all of the blood that arrives in the heart, 85 to 90 percent travels through the body’s network of deep veins.
Given how important these veins are to our circulatory system, it’s easy to see why a deep vein blockage could be very problematic. Deep vein thrombosis occurs when a thrombus forms within a deep vein. In most cases, DVT develops in the patient’s legs, though this condition can also affect veins in the upper body region.
DVT Symptoms
While the clot remains in place, the amount of damage it inflicts on the patient is rather limited. A thrombus that develops in the leg, for example, may cause the patient to feel pain, warmth and/or swelling in this part of the body. On the other hand, the patient may feel perfectly normal; in roughly half of all cases, deep vein thrombosis causes no discernable symptoms.
What makes DVT so dangerous is that thrombi can break off into the bloodstream, traversing up to the heart and eventually winding up in the pulmonary arteries, which transport blood to the lungs. This condition is known as a pulmonary embolism (PE), and it can be fatal if it not properly treated. If a pulmonary embolism does develop, the patient will likely experience several distressing symptoms:
- Shortness of breath
- Difficulty breathing
- Chest pains
- Coughing
- Coughing up blood
If any signs of either deep vein thrombosis or pulmonary embolism do appear, patients are urged to seek immediate medical attention.
Treatment Options
The treatment methods used for DVT are geared towards attaining three goals:
- Prevent current blood clots from increasing in size
- Prevent the clot from breaking off into the bloodstream and reaching the lungs
- Reduce the patient’s risk of suffering a future clot
The most common type of medication given to DVT patients are anticoagulants, a class of drugs also known as blood thinners. Blood thinners are used to prevent new clots from appearing, while also hindering the growth of existing clots in the patient’s bloodstream. Blood thinners are often taken in pill form, but can also be injected underneath the patient’s skin. A third type of blood thinners are given intravenously, meaning that they are directly administered into a vein via a tube or needle.
Blood thinners are generally successful in preventing blood clots and stymieing clot growth. However, anticoagulants are not able to destroy preexisting clots; in many cases, the body takes care of such clots on its own. In addition, blood thinners are not without side effects; sometimes, these drugs do their job too well, and the patient begins to experience problems with bleeding. Given that this issue can be life-threatening, people taking blood thinners typically undergo routine blood testing. These tests are used to measure the clotting capabilities of the patient’s blood.
Some people are unable to take blood thinning medications. As an alternative to blood thinners, these patients might be given a specific type of filter. This filter is inserted into the inferior vena cava, a large vein that carries de-oxygenated blood from the lower body back to the heart. Because of this, these devices are usually referred to as vena cava filters. The purpose of vena cava filters is to intercept blood clots before they reach the pulmonary arteries. Though they can prevent pulmonary embolisms from occurring, vena cava filters are not able to block the formation of new clots.
A third type of DVT medication, known as thrombolytics, is used to eliminate large clots that pose an immediate risk to the patient’s health. The side effects of thrombolytics can be very severe, leading to immediate and intense bleeding. Because of this reason, doctors generally don’t use thrombolytics unless the patient’s life is in jeopardy.
Finally, there is also the option of compression stockings, which are used to alleviate swelling in the legs. The design of these stockings – which tightly grips the ankle but exerts less pressure on the area near the knee cap – allows blood to flow smoothly through the legs without hardening. While this product can be purchased without a prescription, there are stronger versions of these stockings that can be obtained with a prescription.
Preventing DVT
Deep vain thrombosis can certainly be a troubling foe, but it isn’t inevitable. There are a number of precautions that can help ward off blood clots.
- In some patients, physical inactivity can allow clots to form in the legs. It doesn’t take that much time for such a scenario to develop; a person who sits still for hours on end during a trip may fall victim to this condition. Exercising the calf muscles is a good way to improve blood circulation in the legs. One such example would be to lift your heels while keeping your toes firmly planted on the ground. You could also invert this technique, raising your toes while letting your heels remain stationary.
- Those with a history of blood clots are well advised to schedule regular checkups with their doctor, and should also faithfully take all prescribed blood clot medications.
- When recuperating from a major illness or surgery, a patient often ends up bedridden for an extended period of time. This lack of movement can allow clots to form in the legs. Provided that your doctor allows for it, try to walk around as soon as possible when recovering from a serious medical setback.
- In addition to all of the other health-related woes they can trigger, it bears mentioning that obesity, high blood pressure and smoking might also cause blood clots. While losing weight, quitting smoking and managing your blood pressure certainly requires much time and effort, achieving these goals greatly improves the body’s long-term health.
 Natural Knowledge 24/7 Educate yourself with nutrition, health and fitness knowledge.
Natural Knowledge 24/7 Educate yourself with nutrition, health and fitness knowledge.